Developed by Abbott, CLEAR is a program based on physician and patient insights, to help patients with PAD get a timely diagnosis followed by appropriate treatment
CLEAR delivers tailor made educational resources to all involved in the PAD referral process:
- Enhance awareness and understanding of PAD
- Facilitate early referral of patients
- Boost networking and collaboration between referring HCPs and vascular specialists
- Provide easy-to-use tools to streamline referral pathway efficiency
- Help prevent PAD progression to CLTI, save patients' limbs and improve quality of life1
- Connect with an Abbott Representative to learn more on how you can get started quickly and simply.
Access further information on PAD for yourself and your patients.
Register to receive a toolkit with these materials and more
- PAD management guidelines that provide the flow of PAD diagnosis and treatment according to current standard-of-care clinical guidelines
- A brochure to help your patients better understand PAD
- Patient-facing posters that highlight PAD risk factors and anatomy for your use in exam rooms
- A PAD risk checklist for your use with patients to assess PAD risk
- A simple guide for descriptions and instructions on how to use all the materials provided

In Their Own Words
SERIES TRAILER |
EPISODE 1 - The Hidden Crisis: Why Traditional Approaches to Amputation Are Not Enough. Take a closer look at the real-world struggles faced by physicians and patients. |
EPISODE 2 - Transforming Lives Through Amputation Prevention and Value-Based Care. Watch how a team of dedicated physicians makes a powerful impact on PAD and CLTI care, with the goal of optimizing patient outcomes. |
EPISODE 3 - The Urgent Need for Amputation Prevention. Hear from a patient who faced the devastating prospect of life-altering amputation and the physician fighting to prevent it. |



Help your patient understand PAD
Patients diagnosed with peripheral artery disease (PAD) are likely to be concerned about their condition and will want to learn all they can about PAD and how it may affect them. PAD is a common disease affecting over 236 million people worldwide3 and presents in 15-20% of people >70 years of age.4
PAD is the presence of atherosclerotic arteries in the lower limbs, which leads to a reduction in blood flow to the extremities.5,6 PAD is associated with significant morbidity and mortality:
- 5-year mortality rate of 33%7
- 1 in 5 risk of MI, stroke, cardiovascular death, or hospitalization within one year8
- Prevalence that increases 2-fold every 10 years9
- Significant impact on health-related quality of life2,10

The information provided is not intended for medical diagnosis or treatment or as a substitute for professional medical advice.
Consult with a physician or qualified healthcare provider for appropriate medical advice.
This material is intended for use with healthcare professionals only.

Conozca más acerca de STOPDAPT 2

Sharing Information, Promoting Understanding:
Resources to Help Your Patients Walk Away from PAD/CLTI

STOPDAPT-3 Trial Design and Randomization11

- ICP con uso exclusivo y planificado de un stent liberador de everolimus (EES, por sus siglas en inglés ) de CoCr (XIENCE™)
- Presencia de paro cardíaco súbito (SCA, por sus siglas en inglés) o ARC-HBR
- Elegible para DAPT (aspirina/inhibidor P2Y12) durante 1 mes.
Diseño del estudio y aleatorización
Grupo 1:
0 a 1 mes: Aspirina + P2Y12 (Prasugrel)
Después de 1 mes: Monoterapia con clopidogrel
Grupo 2:
0 a 1 mes: P2Y12 (Prasugrel)
Después de 1 mes: Monoterapia con clopidogrel
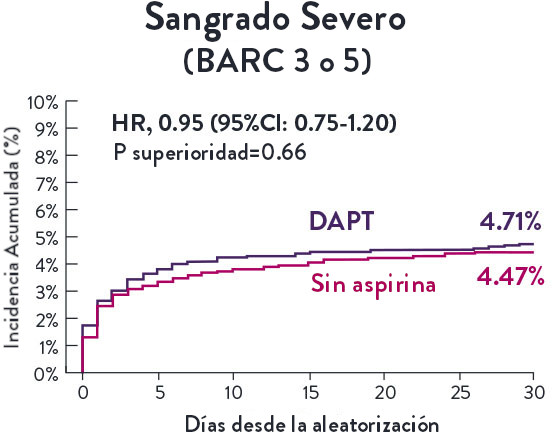
El Ensayo STOPDAPT-311 se diseñó para estudiar la DAPT de 0 meses* (SAPT˄ utilizando solamente un inhibidor P2Y12) para pacientes con paro cardiaco súbito (SCA) y alto riesgo de sangrado (HBR).
Aunque los resultados son comparables tanto para hemorragias como para eventos isquémicos en los brazos de DAPT y TAPS, el estudio no cumplió con su criterio de valoración y concluyó en usar DAPT durante 1 mes después de la ICP.


El stent XIENCE™ sigue siendo el ÚNICO DES con la indicación de DAPT más corta, que puede ser tan corta como 28 días.12


References
1. Walker, C.M., et al. Clin Interv Againg 2015: 10; 1147-1153
2. Wu A, et al. J Am Heart Assoc. 2017; 6(1): e004519.
3. Song P, et al. Lancet Glob Health. 2019; 7(8): e1020-30.
4. Norgren L, et al. J Vasc Surg. 2007; 45(1): S5-67.
5. Hirsch AT, et al. JAMA. 2001; 286(11): 1317-24.
6. Peripheral Arterial Disease (PAD). CDC. Web. 27 Sep 2021.
7. Tomson J, Lip GYH. BMC Cardiovasc Disord. 2005; 5: 15.
8. Steg G, et al. JAMA. 2007; 297(11): 1197-206.
9. Virani SS, et al. Circulation. 2021; 143(8): e254-743.
10. Schorr EN, et al. Geriatr Nurs. 2015; 36(4): 293-300.
11. Duff S, et al. Vasc Health Risk Manag. 2019; 15; 187-208.
12. Conte MS, et al. J Vasc Surg. 2019; 70(2): 662

MAT-XXXXXXX